
Fertility Services
A Wide Variety of Treatment Options at Our Clinics in Scottsdale and Chandler

Initial Evaluation & Diagnosis
Welcome to Bloom! We’re glad to have the opportunity to meet with you during an initial consultation. Your first appointment initiates the evaluation stage, not just for us, but for you as well.
From our perspective, the most important facet of treating infertility is an accurate diagnosis and understanding of underlying causes, of which there could be many. Common causes of infertility include: ovulation or hormonal disorders, uterine or cervical abnormalities, fallopian tube dysfunction or blockage, endometriosis, ovarian insufficiency, pelvic adhesions/scar tissue, uterine fibroids, thyroid problems, and cancer and its treatment. Some not so common causes include: amenorrhea, kidney disease, diabetes, or genetic abnormalities. Male factor causes of infertility can include: abnormal sperm production or function, sperm delivery issues, overexposure to chemicals or toxins, and cancer.
During your initial appointment, Dr. Behera will perform a thorough review of your medical and personal history. She will also address any questions you may have related to your evaluation, the causes of infertility, and all available treatment options. The next step may involve an ultrasound evaluation of the uterus, ovaries and pelvis and physical exam, along with further diagnostic testing for both partners as required based on information gathered from the initial visit. This may include hormone testing, evaluation of fallopian tubes with an hysterosalpingogram test (HSG), and semen analysis for male partners. Finally, Dr. Behera will review your results with you and together, come up with a treatment plan optimized specifically for both your medical and personal fertility needs. (See below for information about the various treatments we offer.)
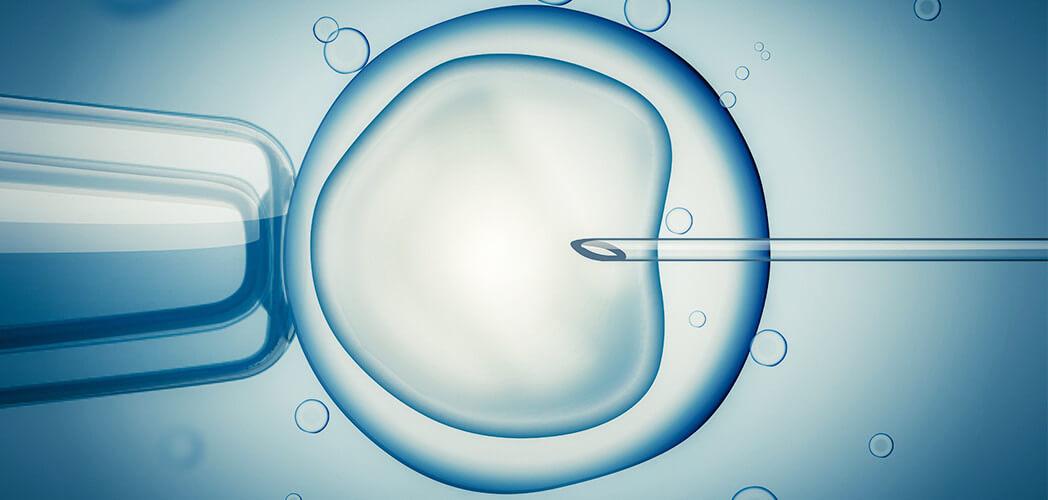
IVF- In-Vitro Fertilization
IVF (In vitro fertilization) is the most common of high-tech fertility treatments. It entails retrieving eggs from ovaries, and fertilizing them with collected sperm in a laboratory. The embryologist monitors and nurtures the fertilized egg (embryo) until it is ready for the physician to transfer into the uterus.
The process usually takes 4-6 weeks per cycle and involves a number of steps.

IUI – Intrauterine Insemination
Intrauterine Insemination (IUI) is a procedure that involves the placement of washed sperm inside a woman’s uterus to assist with conception. It is both, less expensive and less invasive, than IVF. IUI can be very effective for patients with low sperm count, decreased sperm mobility, or unexplained infertility. It is also effective when there are problems with anatomy of the cervix or cervical mucus.
During an IUI, a semen sample is “washed” so that a concentration of optimal sperm can be used for the procedure. For the best IUI outcome, coordination of ovulation timing is everything. The goal is to expose the egg to the best sperm at the right time. Hence, the woman is closely monitored during the cycle for optimal timing and signs of ovulation before IUI is performed. Most often, the precision of ovulation is planned with the administration of an ovulation “trigger” medication (hCG).
Approximately 36 hours after the ovulation trigger, the IUI is performed. Concentrated sperm is placed in the uterus through a soft catheter so that it gets a jump start on its course to the egg for fertilization within the fallopian tube.

Genetic Testing
Preimplantation Genetic Testing (PGT) involves testing embryos for genetic or chromosomal disorders. Tests are conducted at the embryo stage, and require an analysis of cells. Biopsies are conducted on the embryos at the blastocyst stage (day 5), taking a sample of cells from the trophectoderm, which is a precursor to the placenta. The remaining cells of the embryo are left unharmed. Typically, the embryo is then frozen for future transfer, and will not be thawed until results can be reviewed by both the physician and patient.
PGT-A is a screening of the number of chromosomes found in the embryo. Essentially, it alerts us to chromosomal disorders such as Down’s syndrome or Edward’s syndrome.
PGT-M is a test to evaluate single gene disorders in the embryo. Single gene disorders include: cystic fibrosis, hemophilia, Huntington’s disease, Marfan’s disease, muscular dystrophy, thalassemia, Tay Sachs, spinal muscular atrophy, and sickle cell anemia to name a few.

Egg Freezing & Fertility Preservation
Fertility preservation involves the cryopreservation (freezing) of eggs, sperm, or embryos for patients who are concerned about future fertility. The frozen tissue will be stored in liquid nitrogen tanks at lower than 300 degrees below zero (Fahrenheit) to later be used for in vitro fertilization (IVF) or intrauterine insemination (IUI) treatments.
A number of factors can lead to the desire for fertility preservation, including:
- The onset of cancer and other severe diseases
- The effects of the treatment of cancer (chemotherapy or radiation)
- Other severe diseases affecting fertility (endometriosis, lupus, autoimmune disorders) Surgical impact on reproductive organs
- Delaying child bearing for social reasons (career, lifestyle, etc.)
- Advancing age
The technology for fertility preserving treatments has advanced significantly over the last few years. Our IVF embryology team at Bloom Reproductive Institute is highly skilled and knowledgeable in the latest techniques, including vitrification (freezing) of eggs and embryos with high success.

Fertility Enhancing Surgery
At times, specific conditions can contribute to a patient’s infertility and may require surgical intervention. Such conditions include:
- Tubal blockage/obstruction
- Uterine fibroids
- Endometriosis
- Pelvic adhesions
- Uterine or vaginal anatomic variants
- Ovarian cysts
- Intra-uterine adhesions
Dr. Behera specializes in minimally invasive surgical methods to enhance the patient’s fertility. She is highly skilled in the area of advanced laparoscopic surgery, operative hysteroscopy, and robotic surgery. Minimally invasive surgery offers a number of advantages over traditional surgery. They include:
- Shorter recovery times

Donor Egg Program
Bloom’s donor egg program is another option for those patients faced with infertility due to egg factors. This includes women who have suboptimal egg quality or reduced egg number (decreased ovarian reserve), ovarian failure, or haven’t had success with other fertility treatments. It involves taking the eggs from a donor, fertilizing them with a partner’s or donor’s sperm, and then transferring the resulting embryo into the patient.
Success rates for donor egg cycles are significantly higher than traditional IVF for patients with egg factor infertility.
Egg donors, either known or anonymous, are thoroughly screened prior to donation according to the guidelines set forth by the FDA and ASRM. They are screened for personal, family, social, medical, and genetic history. Typical items we screen for include: HIV, hepatitis, STD’s, drug use, infectious disease, psychological issues, and genetic abnormalities.
Once a match has been selected, the reproductive cycles are synchronized for both donor and patient. The donor will go through the IVF process up through the egg retrieval stage, while the recipient will prepare the uterus and continue the process from the embryo transfer stage onward. Many times, we may plan for the egg donor to complete the treatment cycle in advance, and the resulting embryos are frozen. Once the outcome of the cycle is reviewed by the recipient couple, including number and quality of embryos, they may schedule the implantation phase of the cycle at a later date of their choice.

Become an Egg Donor
Egg donation is a magnificent gift to give a couple! Through egg donation, donors provide willing parents the ability to have children. Egg donors are essentially making dreams come true.
In order to become an egg donor, the candidate must go through a screening process according to guidelines established by the Food and Drug Administration (FDA) and American Society for Reproductive Medicine (ASRM). Once passing the screening process, donor candidates undergo fertility treatment, specifically the IVF process, up through the egg retrieval stage. Donor candidates that do pass screening are compensated for their gift of eggs. Egg donation is an anonymous process, where the identity of donors is protected.
Text us at (480) 434-6565 to learn more about our Egg Donation Program.
 Book an Appointment
Book an Appointment  Patient Portal
Patient Portal 







